No, inhaled Lasix isn’t a standard COPD treatment. Oral Lasix (furosemide) is used to manage fluid buildup, a potential complication of severe COPD exacerbations. However, inhaling it presents significant challenges and risks, lacking the efficacy and safety profile of established inhaled therapies.
Focusing on effective COPD management, consider bronchodilators like albuterol or ipratropium for immediate relief and long-acting bronchodilators such as tiotropium or umeclidinium for ongoing maintenance. Inhaled corticosteroids, such as fluticasone or budesonide, can reduce inflammation. These medications are delivered directly to the lungs, offering targeted treatment with better tolerability.
Always consult your physician before initiating or altering any medication regimen. They can assess your specific needs, considering your individual COPD severity and any other health conditions, to devise a personalized treatment plan. Improper medication use carries risks; seeking professional guidance ensures safety and optimizes your chances for successful COPD management.
Consider these points when discussing treatment options with your doctor: Your current symptoms, the frequency of exacerbations, your response to prior treatments, and any potential side effects you’ve experienced. This information helps them select the most appropriate medications and dosages for your situation.
- Inhaled Lasix for COPD: A Detailed Overview
- Alternative Treatment Strategies
- Managing Fluid Retention in COPD
- Potential Risks of Oral Lasix in COPD
- Consult your physician
- Research and Future Directions
- Understanding COPD and Fluid Retention
- Recognizing the Signs
- Managing Fluid Retention in COPD
- Medications
- Regular Monitoring
- When to Seek Immediate Medical Attention
- The Mechanism of Lasix (Furosemide)
- Why Inhaled Administration Might Be Considered
- Reduced Systemic Side Effects
- Improved Pulmonary Delivery
- Potential for Better Patient Compliance
- Future Research Directions
- Evidence Supporting Inhaled Lasix for COPD (or Lack Thereof)
- Oral Lasix in COPD Management
- Reasons for Lack of Inhaled Lasix Use in COPD
- Alternative Treatments for COPD
- Conclusion
- Potential Advantages and Disadvantages of Inhaled Lasix
- Alternative Treatments for Fluid Retention in COPD
Inhaled Lasix for COPD: A Detailed Overview
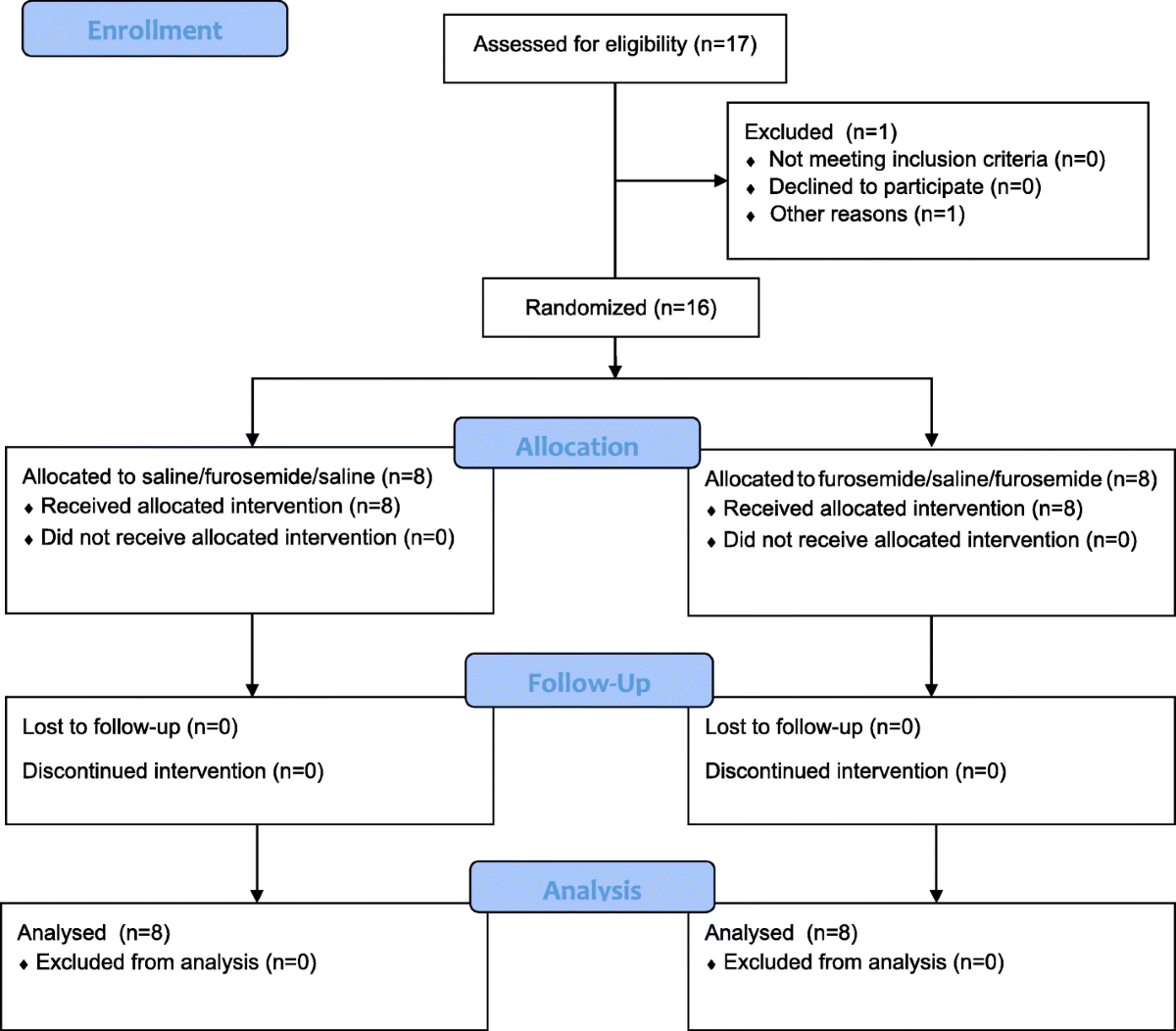
Currently, there is no FDA-approved inhaled formulation of Lasix (furosemide) for COPD treatment. Oral Lasix is sometimes used to manage fluid retention in patients with severe COPD and heart failure, but its use is carefully considered due to potential side effects.
Alternative Treatment Strategies
The cornerstone of COPD management focuses on bronchodilators (like albuterol and tiotropium) and inhaled corticosteroids to reduce inflammation. Pulmonary rehabilitation programs significantly improve exercise capacity and quality of life. Oxygen therapy is crucial for patients with low blood oxygen levels. In cases of severe fluid overload contributing to COPD exacerbation, doctors may prescribe oral diuretics like Lasix, but always under close medical supervision.
Managing Fluid Retention in COPD
Fluid retention, while a potential complication in COPD, isn’t directly treated with inhaled medication. Instead, physicians assess the underlying cause. Heart failure often coexists with COPD, making fluid management complex. Careful monitoring of weight, blood pressure, and fluid intake is necessary. Dietary modifications, such as reducing sodium intake, may also play a significant role.
Potential Risks of Oral Lasix in COPD
Oral Lasix, while effective in removing excess fluid, carries risks, including electrolyte imbalances (low potassium, magnesium), dehydration, and dizziness. These risks are particularly relevant in patients with COPD who may already have fragile health. Therefore, using Lasix requires close monitoring of kidney function and electrolyte levels.
Consult your physician
Always consult your doctor before starting or changing any medications, including diuretics. They will assess your specific condition, consider potential drug interactions, and determine the safest and most effective treatment plan for your COPD.
Research and Future Directions
Ongoing research explores novel therapies for COPD, focusing on targeted treatments addressing underlying mechanisms of the disease. While an inhaled form of Lasix for COPD remains unlikely due to the drug’s properties, innovative approaches may yield alternative inhaled medications to manage fluid retention in the future.
Understanding COPD and Fluid Retention
COPD restricts airflow, impacting the heart’s ability to pump efficiently. This can lead to fluid buildup, or edema, most noticeably in the legs and ankles. However, fluid can also accumulate in the lungs (pulmonary edema), a serious complication.
Recognizing the Signs
Watch for swelling in your lower extremities. Shortness of breath, even at rest, and a persistent cough are also warning signs. Weight gain, despite a decreased appetite, is another important indicator.
Managing Fluid Retention in COPD
Your doctor will likely recommend lifestyle changes, including reducing sodium intake to decrease fluid retention. Dietary adjustments, such as limiting fluids, can be beneficial. Regular, moderate exercise, as advised by your physician, supports better circulation and heart function.
Medications
Medication plays a crucial role. Diuretics (water pills) remove excess fluid from the body. Your doctor will determine the appropriate type and dosage. Oxygen therapy often helps alleviate breathlessness associated with fluid buildup. Strictly follow your prescribed medication regimen.
| Symptom | Possible Cause | Action |
|---|---|---|
| Swelling in legs and ankles | Heart struggling to pump blood efficiently | Contact your doctor; reduce sodium intake |
| Shortness of breath | Fluid in the lungs | Seek immediate medical attention; use prescribed inhalers |
| Weight gain | Fluid retention | Discuss with your doctor; monitor fluid intake |
Regular Monitoring
Regular checkups with your doctor are key. They’ll monitor your condition, adjust medication as needed, and provide support. Open communication with your healthcare team allows for proactive management of your COPD and fluid retention.
When to Seek Immediate Medical Attention
Seek immediate medical care if you experience sudden, severe shortness of breath, chest pain, or significant swelling.
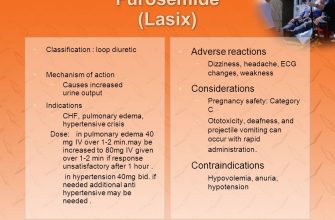
The Mechanism of Lasix (Furosemide)
Lasix, or furosemide, powerfully inhibits sodium and chloride reabsorption in the ascending loop of Henle. This blockage prevents the kidneys from reabsorbing water, leading to increased urine production (diuresis). The increased excretion of sodium and water subsequently lowers blood volume and pressure.
Specifically, furosemide acts on the Na+/K+/2Cl− cotransporter. By binding to this transporter, it directly blocks the movement of sodium, potassium, and chloride ions into the renal tubule cells. This action significantly increases the amount of sodium, potassium, and chloride ions that remain in the tubular fluid and are excreted in the urine.
This diuresis, coupled with the associated reduction in blood volume, is what accounts for Lasix’s impact on symptoms related to fluid overload. It’s important to note that furosemide also increases the excretion of calcium and magnesium.
Caution: While effective, Lasix can cause significant electrolyte imbalances. Careful monitoring of potassium, sodium, and magnesium levels is vital during treatment.
Remember to consult with your healthcare provider for proper diagnosis and treatment. They can provide personalized advice based on your individual medical history and current health status.
Why Inhaled Administration Might Be Considered
Inhaled Lasix offers a targeted approach, delivering the medication directly to the lungs. This minimizes systemic side effects, a significant advantage for COPD patients who are often already taking multiple medications.
Reduced Systemic Side Effects
Oral Lasix, while effective, can cause unwanted effects like dehydration, dizziness, and electrolyte imbalances. Inhaled delivery reduces the amount of Lasix entering the bloodstream, thus potentially mitigating these issues. Studies are needed to definitively quantify this benefit.
Improved Pulmonary Delivery
The primary goal in COPD is improved lung function. An inhaled formulation might achieve higher concentrations of Lasix in the affected lung tissue, leading to potentially more effective fluid removal directly where it’s needed. This targeted approach warrants further investigation.
Potential for Better Patient Compliance
Inhaled medications can be easier for some patients to use compared to oral medications. Improved adherence might translate into better treatment outcomes. Further research should assess this factor.
Future Research Directions
Currently, inhaled Lasix isn’t a standard treatment for COPD. However, the potential benefits mentioned above make it a compelling area for further research. Clinical trials are required to evaluate efficacy and safety profiles compared to existing treatments.
Evidence Supporting Inhaled Lasix for COPD (or Lack Thereof)
Current evidence does not support the use of inhaled Lasix (furosemide) for COPD. While Lasix is a potent diuretic, its primary mechanism of action–increasing sodium and water excretion–doesn’t directly address the underlying pathophysiology of COPD, which involves airway inflammation and airflow limitation.
Oral Lasix in COPD Management
Oral Lasix finds application in managing fluid overload in patients with COPD and concomitant heart failure, a common comorbidity. However, this is distinct from using inhaled Lasix for direct COPD treatment.
Reasons for Lack of Inhaled Lasix Use in COPD
- Lack of clinical trials: No robust clinical trials demonstrate the efficacy and safety of inhaled furosemide for improving lung function or symptoms in COPD patients.
- Pharmacokinetic limitations: Inhaled furosemide may exhibit poor pulmonary absorption. Effective delivery to the target sites in the lungs to elicit a therapeutic effect remains questionable.
- Potential adverse effects: Inhaled furosemide could cause respiratory irritation and exacerbate existing cough. The potential for systemic side effects, such as electrolyte imbalances, also needs careful consideration.
Alternative Treatments for COPD
- Bronchodilators: These medications relax the airway muscles, improving airflow.
- Inhaled corticosteroids: These reduce inflammation in the airways.
- Phosphodiesterase-4 inhibitors: These reduce airway inflammation and improve mucus clearance.
- Oxygen therapy: Improves blood oxygen levels.
- Pulmonary rehabilitation: Improves exercise capacity and quality of life.
Conclusion
In summary, there’s no scientific basis for using inhaled Lasix for COPD. Current treatment guidelines prioritize therapies that specifically target the pathophysiological mechanisms of COPD. Always consult your physician for appropriate COPD management.
Potential Advantages and Disadvantages of Inhaled Lasix
Currently, inhaled Lasix isn’t a standard treatment for COPD. Research into this delivery method is limited. However, hypothetically, inhaled administration could offer several benefits.
Potential Advantages: Faster onset of action compared to oral or intravenous routes could be a significant advantage in managing acute exacerbations. Localized delivery to the lungs might reduce systemic side effects, such as hypotension and electrolyte imbalances, which are common with systemic Lasix. This targeted approach could potentially improve treatment efficacy by directly addressing pulmonary edema contributing to COPD exacerbation.
Potential Disadvantages: Inhaled Lasix faces considerable challenges. Developing a stable, effective inhaled formulation presents a major hurdle. Lasix’s inherent properties make it difficult to aerosolize effectively. Additionally, pulmonary delivery might not achieve sufficient systemic absorption for effective diuresis in all patients. Furthermore, the risk of local irritation or allergic reactions in the lungs remains a concern. Finally, long-term safety data on inhaled Lasix are lacking.
Recommendation: While the theoretical benefits of inhaled Lasix are intriguing for COPD management, further research is needed to confirm its safety and efficacy. Currently, established treatments remain the preferred approach for managing COPD and its associated complications.
Alternative Treatments for Fluid Retention in COPD
Managing fluid retention in COPD often requires a multi-pronged approach. Beyond inhaled medications, several strategies can help.
- Dietary Changes: Reduce sodium intake significantly. Aim for less than 2,000 milligrams per day. Limit processed foods, fast food, and canned goods. Increase potassium-rich foods like bananas and leafy greens to help balance electrolytes. Drink plenty of water, unless specifically advised otherwise by your doctor.
- Medication Adjustments: Your doctor might adjust your diuretic dosage or prescribe additional medications. This may include other diuretics with different mechanisms of action or medications targeting the underlying cause of fluid retention. Always follow your doctor’s instructions precisely.
- Oxygen Therapy: Supplemental oxygen can improve breathing and reduce the strain on your heart, lessening fluid buildup. Discuss oxygen therapy options with your physician if needed.
- Regular Exercise: Gentle exercise, such as walking or cycling, can improve circulation and help manage fluid retention. Always consult your doctor before starting any new exercise program.
- Compression Stockings: Compression stockings can aid in circulation and reduce swelling in the legs and ankles. A doctor or physical therapist can help you find the right fit and compression level.
- Elevation: Elevating your legs when resting can reduce fluid pooling in the lower extremities, thus providing relief from swelling.
Remember, these are potential strategies, and your doctor should guide treatment decisions based on your specific condition and health history. Regular follow-up appointments are crucial for monitoring progress and adjusting treatment as needed.
- Consult your physician before making any changes to your medication or diet.
- Report any worsening symptoms immediately. This includes increased shortness of breath, swelling, or weight gain.