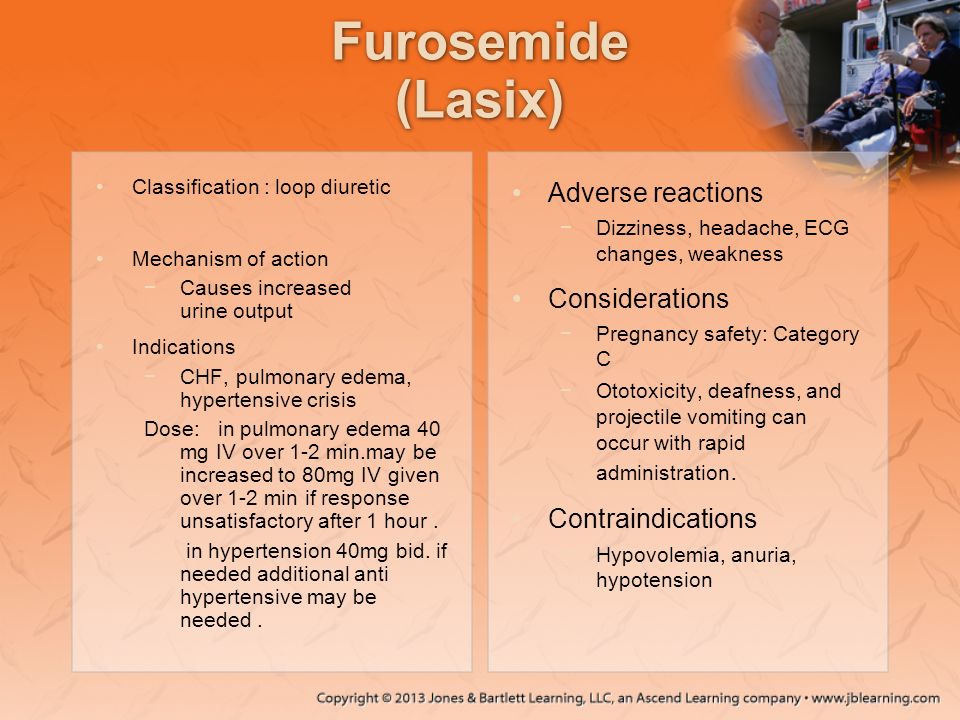
Before starting furosemide, carefully review your medical history. This potent diuretic is contraindicated in individuals with known hypersensitivity to furosemide or other sulfonamide-derived drugs. A history of severe electrolyte imbalances, such as profound hypokalemia or hyponatremia, also necessitates avoiding this medication.
Certain kidney conditions pose significant risks. Furosemide should be used cautiously, or avoided entirely, in patients with severe renal impairment, anuria (absence of urine production), or hepatic coma. Pre-existing conditions like severe dehydration or hypovolemia significantly increase the risk of adverse events and warrant careful consideration before prescribing furosemide.
Specific caution is advised for individuals with gout, as furosemide can elevate uric acid levels, potentially exacerbating gout symptoms. Similarly, patients with diabetes should monitor their blood glucose closely as furosemide can affect glucose tolerance. Finally, pregnant or breastfeeding women should discuss the risks and benefits with their physician before using furosemide, as it can cross the placental barrier and enter breast milk. Always inform your doctor about all medications you’re taking, including over-the-counter drugs and supplements, to minimize potential drug interactions.
Remember: This information is not a substitute for professional medical advice. Always consult your doctor or pharmacist for personalized guidance on furosemide use.
- Contraindications of Furosemide: Severe Renal Impairment
- Increased Risk of Toxicity
- Dosage Adjustments
- Alternative Diuretics
- Contraindications of Furosemide: Electrolyte Imbalances
- Hypokalemia Management
- Other Electrolyte Imbalances
- Monitoring and Adjustment
- Patient Education
- Contraindications of Furosemide: Hepatic Coma and Dehydration
- Hepatic Coma
- Dehydration
- Managing Risk
- Alternative Treatment Options
Contraindications of Furosemide: Severe Renal Impairment
Furosemide should be avoided in patients with severe renal impairment. This is because the kidneys are the primary route of furosemide excretion. Reduced kidney function significantly impairs the body’s ability to eliminate the drug, leading to a build-up of furosemide in the bloodstream.
Increased Risk of Toxicity
This accumulation increases the risk of ototoxicity (hearing damage), nephrotoxicity (kidney damage), and electrolyte imbalances, such as dangerously low potassium levels (hypokalemia). Careful monitoring of serum creatinine and electrolyte levels is needed for patients with even mild-to-moderate renal impairment before considering furosemide use. The dosage should be adjusted, possibly significantly reduced, or an alternative diuretic considered.
Dosage Adjustments
The specific dosage adjustment depends on the severity of renal impairment, often guided by creatinine clearance or estimated glomerular filtration rate (eGFR). Consult prescribing information and guidelines for precise recommendations, and always individualize treatment based on the patient’s overall health status.
Alternative Diuretics
If furosemide is contraindicated due to severe renal impairment, alternative diuretics with different excretion pathways, such as loop diuretics with a lower risk of accumulation in renal failure or thiazide diuretics (if kidney function allows), should be explored. Consult a nephrologist or other specialist for guidance on optimal management of fluid balance in these patients.
Contraindications of Furosemide: Electrolyte Imbalances
Furosemide’s potent diuretic action significantly impacts electrolyte levels, making pre-existing imbalances a serious contraindication. Low potassium (hypokalemia) is a major concern. Severe hypokalemia can trigger life-threatening arrhythmias. Regular potassium level monitoring is crucial during furosemide therapy, especially in patients with conditions predisposing them to hypokalemia, such as kidney disease or those taking other potassium-depleting drugs.
Hypokalemia Management
Potassium supplements may be necessary to counteract furosemide-induced hypokalemia. Dietary adjustments, including increased potassium intake from fruits and vegetables, are also helpful. However, potassium supplementation requires careful medical supervision due to the risk of hyperkalemia. The doctor will determine the appropriate dosage and frequency.
Other Electrolyte Imbalances
Besides potassium, furosemide can also lower levels of magnesium and calcium. Magnesium deficiency can lead to muscle weakness and cramps, while hypocalcemia can cause muscle spasms and cardiac arrhythmias. Monitoring these electrolytes and addressing any deficiencies is vital. Sodium depletion (hyponatremia) is another possibility; careful monitoring and appropriate fluid management are important considerations.
Monitoring and Adjustment
Regular blood tests should assess electrolyte levels throughout furosemide treatment. Dosage adjustments or discontinuation may be necessary based on these results. Close monitoring is particularly important for patients with pre-existing cardiac conditions, liver disease, or those taking other medications that affect electrolyte balance. Prompt medical attention is required for any signs of electrolyte imbalance.
Patient Education
Patients should be fully informed about the potential for electrolyte disturbances. They should be instructed to report any symptoms, such as muscle weakness, cramps, palpitations, or irregular heartbeat. Understanding the importance of regular blood tests and adhering to the prescribed medication regimen are critical for minimizing risks associated with furosemide use.
Contraindications of Furosemide: Hepatic Coma and Dehydration
Furosemide, a potent diuretic, is contraindicated in patients with hepatic coma and severe dehydration. These conditions present unique risks when combined with furosemide’s diuretic action.
Hepatic Coma
In patients with hepatic coma, the liver’s ability to process waste products is significantly impaired. Furosemide’s increased urine production can exacerbate this by depleting electrolytes, particularly potassium and sodium. These electrolyte imbalances can worsen hepatic encephalopathy, potentially leading to further neurological complications, including coma and death. Avoid furosemide in this patient population.
Dehydration
Furosemide’s primary action is to increase urine output. Administering furosemide to a dehydrated patient will further reduce fluid volume, potentially causing hypotension, renal failure, and circulatory collapse. This is particularly risky for elderly patients and those with pre-existing cardiovascular issues.
- Carefully monitor fluid balance before administering furosemide.
- Consider alternative diuretics or adjust the furosemide dose significantly downward.
- Correct dehydration before considering furosemide.
Managing Risk
Before prescribing furosemide, always thoroughly assess the patient’s hydration status and liver function. Regularly monitor serum electrolyte levels, particularly potassium and sodium, during furosemide treatment. Promptly address any electrolyte abnormalities. Closely observe patients for signs of dehydration or worsening hepatic encephalopathy.
Alternative Treatment Options
If furosemide is contraindicated due to hepatic coma or dehydration, explore alternative diuretics with different mechanisms of action or potentially non-pharmacological interventions for fluid management.
- Consider less potent diuretics.
- Explore fluid management strategies.
- Consult with a specialist.