Consider a slow-release prednisone formulation for prolonged symptom management. This approach minimizes the frequency of dosing and potentially reduces the risk of significant side effects associated with daily high-dose regimens.
Research suggests that long-acting prednisone preparations can offer advantages in conditions requiring extended corticosteroid therapy, such as autoimmune diseases or severe allergies. This delivery method helps maintain consistent blood levels, leading to more predictable therapeutic effects. However, individual responses vary, and close monitoring by your doctor is crucial.
Key benefits may include improved adherence due to reduced pill burden, and potentially less pronounced adrenal suppression. Important considerations include potential variations in absorption rates depending on the specific formulation and individual factors. Always discuss available options and potential risks with your healthcare provider before starting any treatment. They will help tailor the best approach for your specific health needs and medical history.
Remember to inform your doctor about all other medications you are currently taking. Interactions with other drugs may necessitate dosage adjustments or alternative treatment strategies. Open communication with your physician is essential for safe and effective management of your condition.
- Long-Acting Prednisone: A Detailed Overview
- Understanding Prednisone’s Action
- Managing Prednisone Therapy
- Potential Side Effects and Mitigation Strategies
- Tapering Off Prednisone
- Alternative Treatment Options
- Understanding the Difference Between Standard and Long-Acting Prednisone
- Dosage and Administration: A Practical Guide
- Oral Administration
- Important Considerations
- Specific Dosage Examples (Illustrative Only – Not a Prescription)
- Common Side Effects and How to Manage Them
- Managing Other Potential Side Effects
- Potential Interactions with Other Medications
- Gastrointestinal Medications
- Diabetes Medications
- Heart Medications
- Immunosuppressants
- Anticoagulants
- Vaccines
- Other Considerations
- Long-Term Use and its Implications
- Metabolic Changes
- Musculoskeletal Issues
- Other Potential Complications
- Managing Long-Term Prednisone Use
- When to Consult Your Doctor Regarding Long-Acting Prednisone
- Alternative Treatments and Considerations
Long-Acting Prednisone: A Detailed Overview
No long-acting formulation of prednisone exists. Prednisone is rapidly metabolized, requiring daily dosing. However, doctors often prescribe a tapering schedule to minimize withdrawal symptoms.
Understanding Prednisone’s Action
Prednisone works by suppressing the immune system. This makes it effective for treating inflammation in conditions like asthma and arthritis. However, prolonged use carries significant risks, including osteoporosis, weight gain, and increased risk of infection.
Managing Prednisone Therapy
Close monitoring by a physician is crucial. Regular blood tests track potential side effects. Dietary changes, such as increased calcium and vitamin D intake, help mitigate osteoporosis risk. Exercise, particularly weight-bearing activities, supports bone health.
Potential Side Effects and Mitigation Strategies
| Side Effect | Mitigation Strategy |
|---|---|
| Increased risk of infection | Maintain good hygiene, get vaccinations, and report any signs of illness immediately. |
| Weight gain | Focus on a healthy, balanced diet low in processed foods and sugars. |
| Osteoporosis | Increase calcium and vitamin D intake, engage in weight-bearing exercise. |
| Mood changes | Open communication with your doctor, support groups and/or therapy. |
Tapering Off Prednisone
Abrupt cessation can lead to adrenal insufficiency. Your doctor will create a gradual tapering schedule, reducing the dose slowly over time to allow your body to adjust naturally. This process often takes weeks or months.
Alternative Treatment Options
Depending on the condition being treated, alternatives to prednisone might include other corticosteroids, biologics, or non-steroidal anti-inflammatory drugs (NSAIDs). Discuss options with your doctor.
Understanding the Difference Between Standard and Long-Acting Prednisone
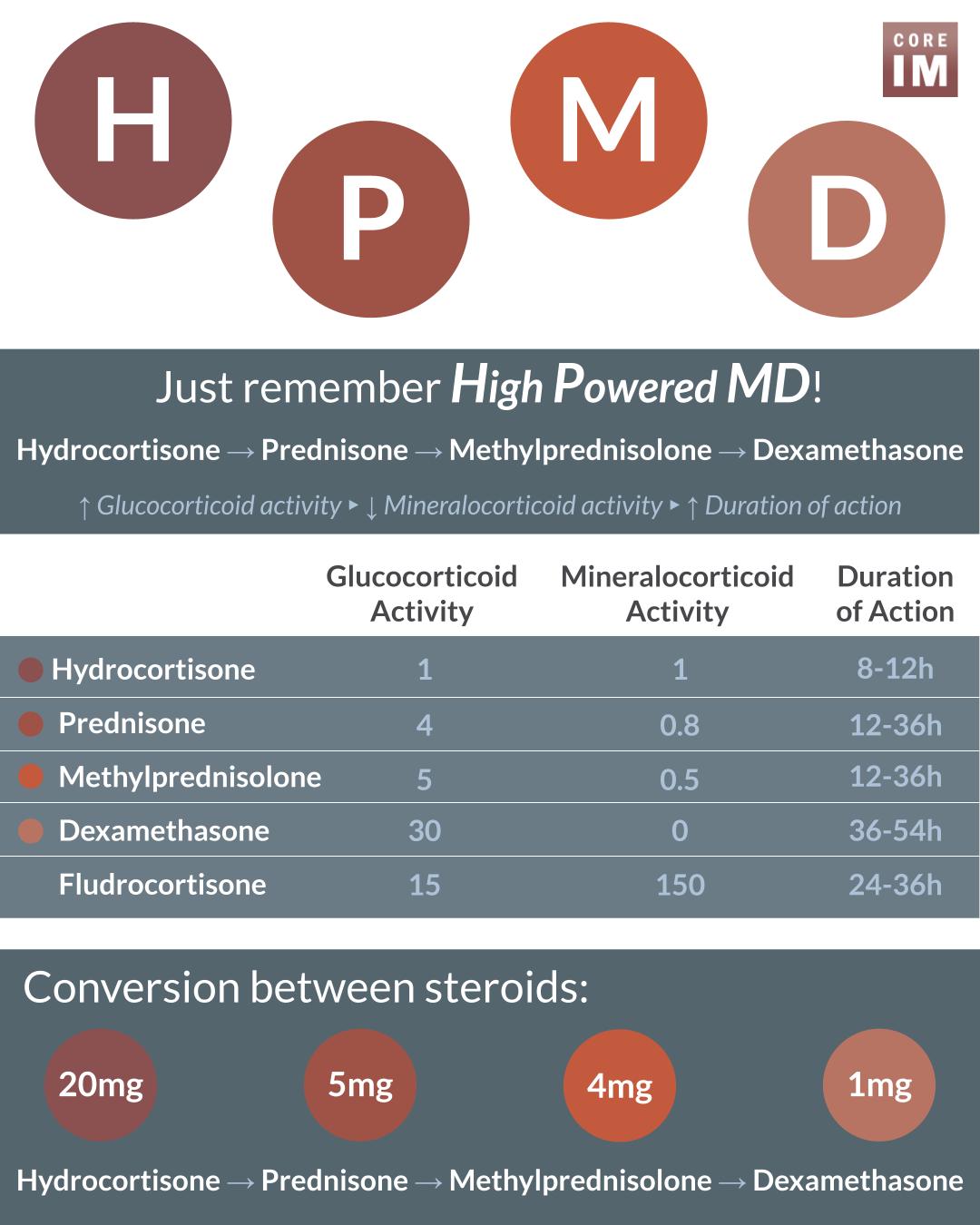
Standard prednisone requires daily dosing, while long-acting formulations, like prednisolone acetate, offer less frequent administration.
- Frequency of Dosing: Standard prednisone usually needs daily administration, sometimes multiple times a day, depending on the dosage and condition. Long-acting options might require injections every few weeks or months, leading to less frequent medication interactions and improved patient adherence.
- Duration of Action: Standard prednisone’s effects are shorter-lived, necessitating consistent daily intake to maintain therapeutic levels. Long-acting versions provide sustained drug levels over an extended period, minimizing fluctuation.
- Side Effects: Both types share potential side effects like weight gain, mood changes, and increased blood sugar. However, the frequency and severity might vary depending on the specific formulation and dosage, and the patient’s individual response.
- Conditions Treated: Both standard and long-acting prednisone treat various inflammatory and autoimmune conditions. The choice depends on the condition’s severity and the desired treatment schedule. For example, long-acting forms are often preferred for conditions requiring prolonged treatment and where frequent dosing presents challenges.
- Administration Routes: Standard prednisone is typically oral. Long-acting forms can be oral, but are often administered via injection (intra-articular, intramuscular, or intravenous) depending on the specific medication and target area.
Remember, a doctor should determine the appropriate prednisone type and dosage. Always discuss potential benefits and risks before starting any medication. This information is for educational purposes only and should not substitute professional medical advice.
- Consult your doctor to determine which prednisone type best suits your individual needs and health status.
- Closely monitor for any side effects and report them immediately to your physician.
- Strictly adhere to your prescribed dosage and administration schedule.
Dosage and Administration: A Practical Guide
Long-acting prednisone dosages vary greatly depending on your specific condition and response to treatment. Your doctor will determine the optimal dosage for you. Never adjust your medication without consulting them.
Oral Administration
Long-acting prednisone is typically administered orally. Follow your doctor’s instructions precisely regarding the timing and frequency of your doses. For example, you might take a single dose daily, or your doctor may prescribe a divided dose, split throughout the day.
- Consistency is key: Take your medication at the same time each day to maintain consistent blood levels.
- Swallowing pills: Swallow the tablets whole with a full glass of water. Do not crush, chew, or break them.
- Missed doses: If you miss a dose, take it as soon as you remember, unless it’s almost time for your next dose. Never double up on doses.
Important Considerations
Your doctor will monitor you closely for side effects. Report any new or worsening symptoms immediately.
- Food Interactions: Some foods and medications can affect how your body absorbs prednisone. Discuss any potential interactions with your doctor or pharmacist.
- Lifestyle Changes: Maintaining a healthy diet and lifestyle is beneficial during treatment. Your doctor may recommend specific dietary changes or exercise routines.
- Tapering Off: Long-acting prednisone should be tapered off gradually under your doctor’s supervision, to minimize withdrawal symptoms. Never stop abruptly.
Specific Dosage Examples (Illustrative Only – Not a Prescription)
- Rheumatoid Arthritis: Initial doses may range from 5-60 mg per day, adjusted according to the patient’s response.
- Lupus: Dosages can vary significantly depending on disease severity and can be adjusted based on individual response.
- Asthma: Starting doses for asthma can range considerably, with adjustments made based on symptom control.
Disclaimer: This information is for educational purposes only and should not be considered medical advice. Always consult your doctor or pharmacist for personalized guidance on dosage and administration of long-acting prednisone.
Common Side Effects and How to Manage Them
Long-acting prednisone, while effective, can cause side effects. Weight gain is common; focus on a balanced diet rich in fruits, vegetables, and lean protein, and incorporate regular exercise. Increased appetite is often linked to weight gain, so mindful eating practices are crucial. Consult a dietitian for personalized guidance.
Managing Other Potential Side Effects
Fluid retention can lead to swelling. Reduce sodium intake, and drink plenty of water. High blood pressure is another possibility; monitor your blood pressure regularly and follow your doctor’s recommendations for medication. Increased blood sugar levels are possible, especially in diabetics. Regular blood sugar monitoring is necessary, and your doctor might adjust your diabetes medication. Mood changes, including irritability or anxiety, are also possible. Open communication with your doctor and family is important. Adequate sleep and stress management techniques can help. Osteoporosis risk increases with long-term use. Discuss bone density testing with your doctor, and consider calcium and vitamin D supplements. Finally, be aware of increased risk of infections. Practice good hygiene and report any signs of infection to your physician immediately.
Remember, these are potential side effects, not guaranteed outcomes. Your doctor can help you understand your individual risk and manage any complications effectively.
Potential Interactions with Other Medications
Long-acting prednisone, like other corticosteroids, can interact significantly with various medications. Always inform your doctor about all medications you are taking, including over-the-counter drugs, supplements, and herbal remedies. This allows your physician to assess potential risks and adjust your treatment accordingly.
Gastrointestinal Medications
Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or naproxen, increase the risk of stomach ulcers and bleeding when combined with prednisone. Your doctor may recommend protective measures like proton pump inhibitors.
Diabetes Medications
Prednisone can raise blood sugar levels, potentially requiring adjustments to your diabetes medications. Close monitoring of your blood glucose is crucial. Your doctor might need to adjust insulin dosages or oral hypoglycemic agents.
Heart Medications
Prednisone can interact with certain heart medications, like digoxin, affecting their effectiveness. Regular monitoring of your heart function is necessary.
Immunosuppressants
Combining prednisone with other immunosuppressants, such as azathioprine or cyclosporine, increases the risk of infections. Your doctor will closely monitor your condition and may adjust dosages.
Anticoagulants
Prednisone can affect the effectiveness of anticoagulants like warfarin. Regular blood tests are required to monitor your INR (International Normalized Ratio) and ensure your blood thins properly.
Vaccines
Avoid receiving live vaccines while taking prednisone as the medication can weaken your immune response, making vaccines less effective. Discuss vaccination plans with your doctor.
Other Considerations
Interactions can also occur with medications affecting potassium levels, bone health, or central nervous system function. Open communication with your healthcare provider ensures safe and effective treatment.
Long-Term Use and its Implications
Long-term prednisone use, exceeding three months, significantly increases the risk of several adverse effects. We recommend close monitoring by your physician.
Metabolic Changes
Prolonged prednisone use often leads to increased blood sugar levels, potentially causing or worsening diabetes. Weight gain, predominantly in the abdominal area, is also common. Increased cholesterol and triglyceride levels contribute to cardiovascular risks. Regular blood tests to monitor these factors are vital.
Musculoskeletal Issues
Osteoporosis, characterized by weakened bones, is a serious concern. Prednisone suppresses bone formation. Muscle weakness and wasting, termed muscle atrophy, can also occur. Regular exercise and a calcium-rich diet can help mitigate these risks, but discuss appropriate exercise regimes with your doctor before starting any new programs.
Other Potential Complications
Infections: Prednisone weakens the immune system, increasing susceptibility to infections. Glaucoma and cataracts: Long-term use can elevate intraocular pressure, increasing the risk of these eye conditions. Mood changes: Anxiety, depression, and insomnia are possible side effects. Skin thinning: The skin becomes more fragile and prone to bruising. Open communication with your doctor regarding any unusual symptoms is critical. Regular check-ups, including eye exams, are recommended.
Managing Long-Term Prednisone Use
Gradual tapering: Stopping prednisone abruptly can be dangerous. Your doctor will create a gradual tapering schedule to minimize withdrawal symptoms. Lifestyle modifications: A balanced diet, regular exercise, and stress management techniques can help mitigate some side effects. Monitoring: Regular blood tests and check-ups are necessary to track your health and adjust medication as needed. Remember to discuss all health concerns with your physician.
When to Consult Your Doctor Regarding Long-Acting Prednisone
Contact your doctor immediately if you experience any new or worsening symptoms, especially severe headaches, vision changes, increased thirst or urination, rapid weight gain, easy bruising or bleeding, persistent nausea or vomiting, or significant mood swings. These could indicate serious side effects.
Schedule a follow-up appointment as soon as possible if you notice any changes in your blood pressure, blood sugar levels, or cholesterol. Regular monitoring is key while taking long-acting prednisone.
Report any infections, no matter how minor, to your doctor. Prednisone can weaken your immune system, making you more vulnerable.
Discuss any medication changes with your doctor before adjusting your prednisone dosage or stopping the medication abruptly. Sudden cessation can lead to serious complications.
If you experience muscle weakness, bone pain, or fragility, inform your doctor. Long-term prednisone use can increase the risk of osteoporosis and muscle wasting.
Always communicate openly and honestly with your doctor about any concerns or questions you may have regarding your treatment. Their guidance is vital for your health and well-being.
Note: This information is for guidance only and does not replace professional medical advice. Always consult your physician for personalized care.
Alternative Treatments and Considerations
Explore non-steroid options like biologics, such as infliximab or adalimumab, for managing inflammation. These medications target specific components of the immune system, offering a different approach than corticosteroids.
Consider disease-modifying antirheumatic drugs (DMARDs), including methotrexate or sulfasalazine, for long-term management of underlying inflammatory conditions. These drugs help slow disease progression.
Physical therapy can significantly reduce pain and improve joint mobility. A customized program focusing on strengthening and range-of-motion exercises can yield positive results.
Lifestyle changes, including regular exercise, a balanced diet rich in anti-inflammatory foods, and stress management techniques like yoga or meditation, support overall well-being and potentially reduce inflammation.
Always consult your doctor before starting any new treatment. They can assess your specific condition and guide you toward the most appropriate approach, considering potential drug interactions and your overall health. Regular monitoring of blood work helps track treatment efficacy and detect any potential side effects.
Discuss tapering strategies with your physician to minimize the risks associated with long-term corticosteroid use. A gradual reduction in dosage, under medical supervision, is critical for a safe transition.