No, Accutane (isotretinoin) is not safe during breastfeeding. The drug readily passes into breast milk, posing significant risks to the nursing infant.
Studies show high concentrations of isotretinoin in breast milk, potentially causing severe birth defects in the baby. These defects can affect various organs, leading to long-term health complications. Therefore, breastfeeding should be stopped completely if you’re taking Accutane.
Alternative treatments for acne exist that are safer during breastfeeding. Consult your dermatologist and healthcare provider to explore options like topical retinoids, antibiotics, or hormonal therapies. They can help you manage acne effectively while protecting your baby’s health. Open communication with your medical team is vital during this time.
Remember, your doctor can provide personalized guidance and help you create a safe and effective treatment plan. Discuss your concerns openly; they’re there to support you through this period.
- Is Accutane Safe While Breastfeeding?
- Alternatives for Acne During Breastfeeding
- Discussing Treatment Options with Your Doctor
- Comparison of Treatment Options
- Important Note:
- Accutane’s Mechanism of Action and Potential Risks
- Accutane Levels in Breast Milk: What Research Shows
- Risks to the Nursing Infant: Potential Side Effects
- Alternatives to Accutane During Breastfeeding
- Topical Treatments
- Lifestyle Changes
- Oral Antibiotics
- Consulting Your Doctor: Importance of Personalized Advice
- Weighing the Risks and Benefits: A Personalized Decision
- Long-Term Effects on the Child: What We Know and Don’t Know
Is Accutane Safe While Breastfeeding?
No, Accutane (isotretinoin) is not safe to use while breastfeeding. This powerful medication is known to cause severe birth defects, and detectable levels can be present in breast milk. The risk to your baby significantly outweighs any potential benefits.
Alternatives for Acne During Breastfeeding
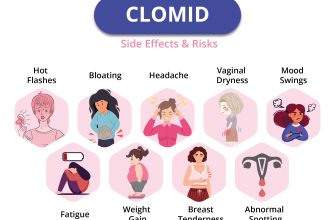
Many effective acne treatments are available that are considered safe for breastfeeding mothers. These options include topical retinoids (like tretinoin, but at a lower concentration than Accutane), topical antibiotics, and benzoyl peroxide. Your dermatologist can help you find the best approach for your specific skin type and condition.
Discussing Treatment Options with Your Doctor
It’s crucial to have an open conversation with your doctor or dermatologist about your acne and breastfeeding goals. They can assess your individual circumstances and recommend a suitable treatment plan. They’ll consider the severity of your acne, your overall health, and the potential risks and benefits of various treatment options.
Comparison of Treatment Options
| Treatment | Safe During Breastfeeding? | Effectiveness for Acne |
|---|---|---|
| Accutane (Isotretinoin) | No | Very High |
| Topical Retinoids (low concentration) | Generally Yes | Moderate |
| Topical Antibiotics | Generally Yes | Moderate |
| Benzoyl Peroxide | Yes | Moderate |
Important Note:
Always follow your doctor’s instructions regarding any medication you use while breastfeeding. Never self-medicate. Regular check-ups with your doctor will help monitor your progress and make adjustments to your treatment plan as needed.
Accutane’s Mechanism of Action and Potential Risks
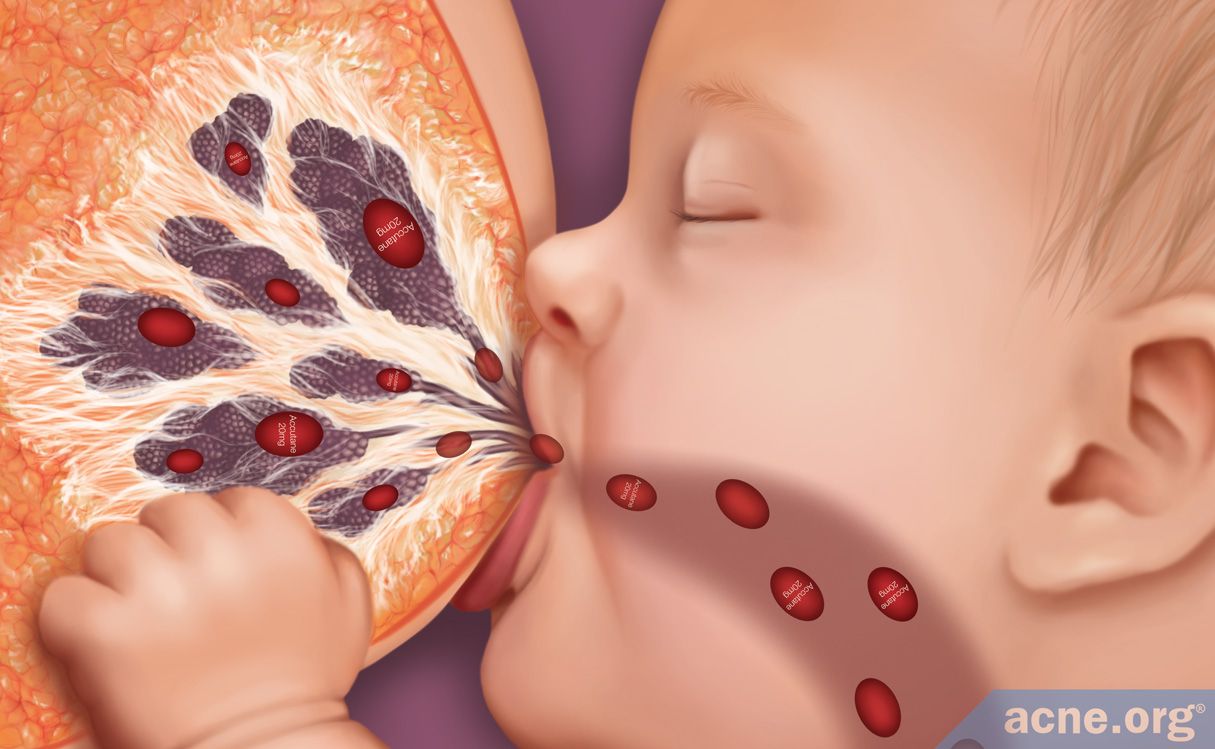
Accutane, or isotretinoin, powerfully reduces sebum production by binding to retinoic acid receptors in sebaceous glands. This significantly decreases oil production, a key factor in acne development. It also reduces inflammation and helps prevent the formation of new comedones (blocked pores).
However, isotretinoin’s potent effects carry potential risks. Teratogenicity is a major concern. Isotretinoin causes severe birth defects, including facial abnormalities and heart defects, if taken during pregnancy. Therefore, pregnancy prevention is paramount for anyone considering or using this medication.
Other potential side effects include dry skin, lips, and eyes; increased risk of depression and suicidal thoughts; elevated blood lipid levels; and liver abnormalities. Regular blood tests monitor liver function and lipid levels. Mental health monitoring is also crucial.
Rare, but serious, side effects include pancreatitis and inflammatory bowel disease. Immediate medical attention is required if severe abdominal pain occurs. The medication also increases sun sensitivity; using a high SPF sunscreen is strongly recommended.
Because isotretinoin passes into breast milk, the recommendation is to avoid breastfeeding while taking Accutane to minimize infant exposure to the drug and its potential consequences. This decision requires discussion with both a dermatologist and an obstetrician or a family doctor.
Accutane Levels in Breast Milk: What Research Shows
Studies show isotretinoin (Accutane) does transfer into breast milk, though at very low concentrations. One study measured isotretinoin levels in breast milk averaging 0.02 ng/mL after a single dose. This is significantly lower than therapeutic levels used to treat acne.
Another study found that even with consistent Accutane use, the amount transferred to breast milk remains minimal, posing a negligible risk to the infant. However, individual results can vary.
While risk appears low based on current research, doctors generally recommend avoiding breastfeeding while taking isotretinoin as a precaution. This is because long-term effects from low-level exposure are not fully understood. Always consult your doctor for personalized advice.
Mothers should discuss their individual circumstances and medication regimen with their physicians and a lactation consultant to make an informed decision about breastfeeding while using Accutane. Regular monitoring of the infant’s health is advised in cases where breastfeeding continues during Accutane treatment.
Risks to the Nursing Infant: Potential Side Effects
Accutane (isotretinoin) is known to pass into breast milk in small amounts. While the risk to the nursing infant is generally considered low, potential side effects exist, requiring careful consideration.
Studies show isotretinoin levels in breast milk are typically low, and most babies exposed show no apparent adverse effects. However, potential side effects include dryness of the skin and mucous membranes, which might manifest as dry, cracked lips or skin irritation. Infants might also experience slowed growth in some cases. These effects are typically mild and temporary.
The severity of potential side effects depends on factors such as the mother’s dosage, the infant’s metabolism, and the duration of breastfeeding. Monitoring the infant for any unusual skin changes or slowed growth is recommended.
Regular checkups with your pediatrician are crucial to closely monitor the infant’s health and well-being during breastfeeding while the mother is taking Accutane. Open communication with your doctor about any concerns is paramount. They can help you weigh the potential risks against the benefits of breastfeeding.
Remember, individual responses vary. This information aims to provide guidance, not replace professional medical advice. Always consult your healthcare provider before making decisions concerning your medication and breastfeeding.
Alternatives to Accutane During Breastfeeding
Discuss treatment options with your dermatologist. They can help you weigh the risks and benefits of different approaches, considering your specific situation and breastfeeding status. Non-prescription treatments, such as gentle cleansers and moisturizers formulated for sensitive skin, can help manage mild acne.
Topical Treatments
Many topical retinoids, like tretinoin or adapalene, are generally considered safer than Accutane during breastfeeding. However, always consult your doctor before starting any new treatment. Azelaic acid and benzoyl peroxide are additional topical options that may prove beneficial. Remember that efficacy varies between individuals, and your dermatologist can help determine the most suitable option for your skin type and acne severity. Regular application is key for consistent results.
Lifestyle Changes
Simple lifestyle adjustments can significantly impact acne. A balanced diet, reducing stress levels, and maintaining a consistent skincare routine can contribute to clearer skin. These changes may not eliminate acne entirely, but they often support other treatment methods and promote overall well-being. Sufficient sleep and hydration are also vital factors in healthy skin maintenance.
Oral Antibiotics
In some cases, your dermatologist may prescribe oral antibiotics specifically designed for acne. These antibiotics should only be used under strict medical supervision, and your doctor will carefully consider their compatibility with breastfeeding.
Consulting Your Doctor: Importance of Personalized Advice
Always speak with your doctor before making any decisions about medication while breastfeeding. Your health and your baby’s health are paramount.
Your doctor will consider several factors:
- Your specific medical history.
- The severity of your acne.
- Your baby’s age and health.
- Your breastfeeding patterns.
- Available alternatives to Accutane.
They can assess the potential risks and benefits tailored to your unique circumstances. This personalized approach is key.
Expect your doctor to discuss potential side effects, both for you and your baby. This includes monitoring your baby’s development closely.
Don’t hesitate to ask questions! Clarify any concerns about Accutane and breastfeeding. A thorough understanding will empower you to make informed choices.
- Discuss alternative acne treatments that are safe during breastfeeding.
- Inquire about blood tests to monitor your Accutane levels if prescribed.
- Ask about strategies to minimize potential risks if you choose to take Accutane.
- Understand the process for reporting any side effects you or your baby might experience.
Remember, open communication with your doctor is crucial for your wellbeing and your baby’s.
Weighing the Risks and Benefits: A Personalized Decision
Accutane and breastfeeding pose a significant challenge. There’s no simple yes or no answer. Your decision requires careful consideration of individual factors.
First, understand the risks. Accutane, a potent medication, can pass into breast milk, potentially harming your baby. Research suggests the amount transferred is low, but the long-term effects on a nursing infant remain largely unknown. Potential risks for your baby might include birth defects (if you become pregnant while taking Accutane), or developmental issues. These risks are most significant during the first trimester of pregnancy; however, even low levels of exposure can theoretically cause harm. This uncertainty is the core of the difficulty.
- Consult your dermatologist: Discuss your specific skin condition and treatment options. Weigh the severity of your acne against the potential risks to your baby. Your dermatologist can help you assess your individual risk profile.
- Consult your obstetrician or gynecologist: They can provide guidance on the safest course of action, considering your health and your baby’s well-being.
- Consider alternative treatments: Explore other acne treatments compatible with breastfeeding. Your healthcare providers can discuss options like topical retinoids or antibiotics. They can help you make informed choices given your individual circumstances.
Secondly, assess the benefits. Severe acne significantly impacts quality of life. Untreated acne can lead to scarring, psychological distress and low self-esteem. Weigh the potential improvement in your well-being against the potential risks to your child. This is a deeply personal equation.
- Monitor your baby closely: If you choose to continue Accutane while breastfeeding, regular checkups with your pediatrician are crucial for monitoring your baby’s development and identifying any potential issues early.
- Document your decision: Maintain thorough records of your discussions with your healthcare providers, your treatment plan, and any observations about your baby’s health. This detailed documentation provides a valuable resource for future reference and can assist your providers in making well-informed decisions.
- Prioritize open communication: Maintain a consistent dialogue with your medical team and openly discuss any concerns or changes in your baby’s health.
Ultimately, the decision rests solely with you. This detailed weighing of risks and benefits, guided by qualified medical professionals, is the key to making the best decision for you and your child.
Long-Term Effects on the Child: What We Know and Don’t Know
Current research provides limited data on long-term effects of Accutane exposure during breastfeeding. We lack extensive, long-term studies tracking children exposed to isotretinoin via breast milk. This makes definitive statements about long-term consequences challenging.
Studies focusing on Accutane’s presence in breast milk show minimal concentrations, suggesting low risk of direct harm. However, these studies often lack the prolonged follow-up needed to assess potential subtle developmental effects. More research is needed to fully understand potential long-term impacts on the child’s cognitive development, growth, and overall health.
Doctors currently recommend caution and advise mothers to weigh the benefits of breastfeeding against potential, though currently unquantified, risks. Open communication with your doctor about your individual circumstances is paramount. They can help you assess your risk factors and make informed decisions based on your specific situation. This decision should consider the mother’s health needs and the infant’s overall well-being.
Ongoing research aims to fill these knowledge gaps. Future studies employing larger sample sizes and extended follow-up periods will be instrumental in providing clearer guidance on the long-term effects of Accutane exposure through breast milk. Until then, a cautious approach and open communication with your healthcare provider are key.