A 1000 mg prednisone dose is a very high dosage, typically reserved for severe inflammatory conditions requiring rapid and potent immunosuppression. This level of prednisone carries significant risks and should only be administered under strict medical supervision. We’ll explore potential uses, side effects, and vital monitoring needs in detail.
Conditions like severe allergic reactions, certain autoimmune diseases flares, and some forms of organ rejection might necessitate such a high dose. However, it’s crucial to understand that prolonged use at this level is generally avoided due to the considerable potential for adverse events. Expect frequent blood tests to monitor your blood counts and other vital functions. Your doctor will carefully adjust the dosage and duration based on your response and tolerance.
Common side effects at this dosage include significant fluid retention, increased blood sugar, increased risk of infection, mood swings, and insomnia. Less common, yet serious, potential side effects include osteoporosis, cataracts, and increased risk of cardiovascular problems. Open and honest communication with your doctor is paramount to managing these risks and making necessary adjustments to your treatment plan. Regular monitoring allows for early detection and intervention.
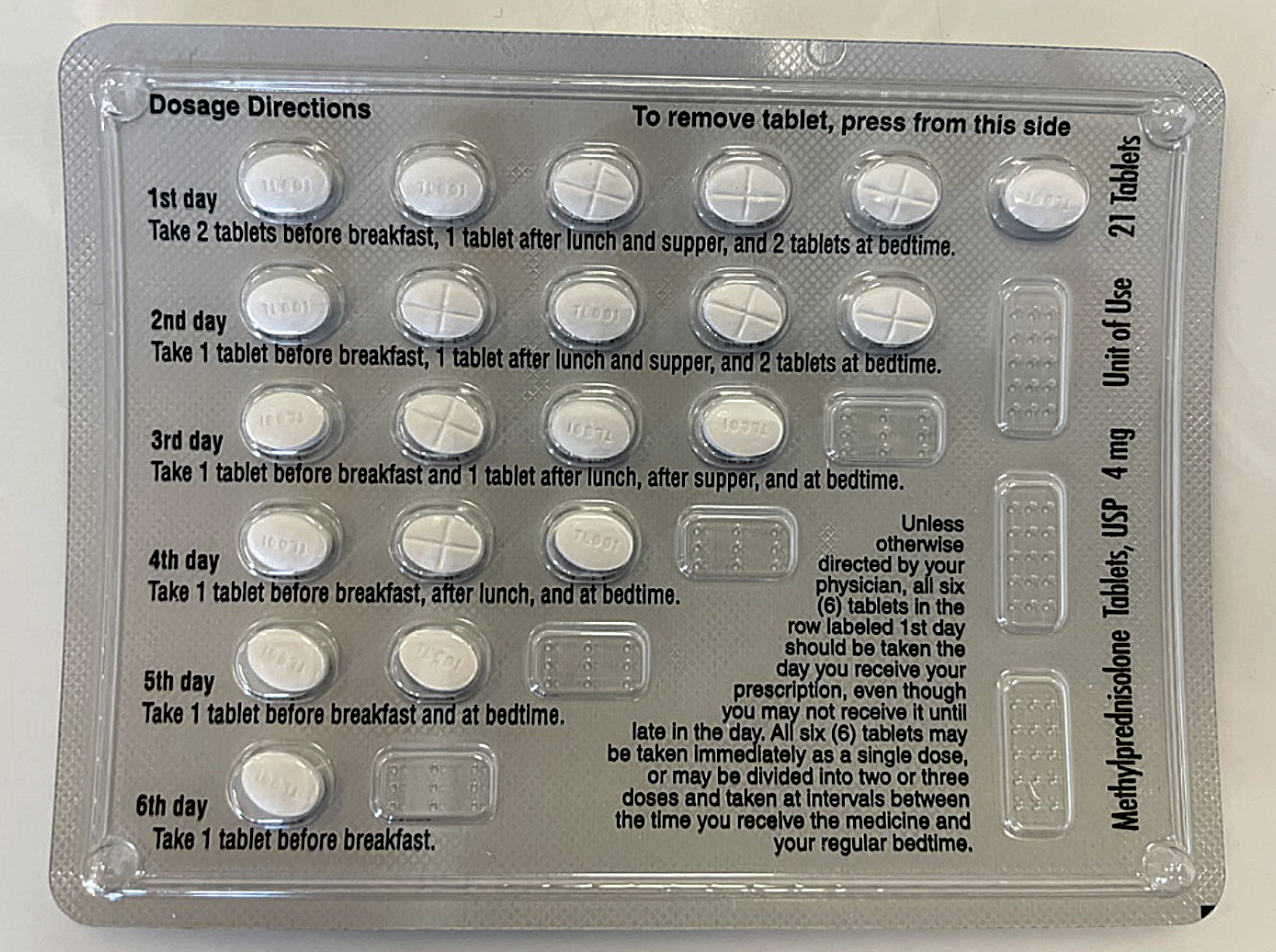
Never adjust your prednisone dosage without explicit instructions from your physician. Sudden cessation of high-dose prednisone can trigger a dangerous rebound effect. The tapering process, carefully managed by your doctor, is crucial for safe discontinuation of treatment. Your healthcare team will guide you every step of the way, ensuring your safety and well-being during and after this high-dose regimen. This information is for educational purposes only and should not replace professional medical advice.
- 1000 mg Prednisone Dose: A Comprehensive Overview
- Potential Uses
- Risks and Side Effects
- Administration and Monitoring
- Alternatives
- Disclaimer:
- Immediate Effects and Short-Term Considerations
- Monitoring Blood Sugar
- Gastrointestinal Upset
- Long-Term Risks and Management of Side Effects
- Withdrawal and Tapering Strategies
- Understanding the Tapering Process
- Potential Withdrawal Symptoms and Management
1000 mg Prednisone Dose: A Comprehensive Overview
A 1000 mg prednisone dose is a very high dose, typically used only in severe cases requiring rapid and intense anti-inflammatory or immunosuppressive effects. This isn’t a routine dosage and carries significant risks.
Potential Uses
Such a high dose might be considered for conditions like severe allergic reactions (anaphylaxis), acute exacerbations of autoimmune diseases (e.g., lupus, severe rheumatoid arthritis), or certain types of cancer treatment.
Risks and Side Effects
High-dose prednisone can cause a wide range of side effects, including: increased blood sugar, weight gain, fluid retention, high blood pressure, insomnia, mood changes (including anxiety and depression), muscle weakness, increased risk of infections, thinning of the skin, and bone loss. Long-term use at high doses raises the risk of serious complications like cataracts, glaucoma, and osteoporosis.
Administration and Monitoring
A 1000 mg prednisone dose is usually given intravenously in a hospital setting under close medical supervision. Doctors carefully monitor patients for side effects and adjust the dosage as needed. Tapering off the medication gradually is crucial to minimize withdrawal symptoms. Regular blood tests are frequently required to track blood sugar, electrolytes, and other vital indicators.
Alternatives
Other medications may be suitable depending on the specific condition. Your physician will discuss the benefits and risks of alternative treatment options before prescribing such a high dose of prednisone.
Disclaimer:
This information is for educational purposes only and does not constitute medical advice. Always consult your doctor or other qualified healthcare professional before making any decisions related to your health or treatment.
Immediate Effects and Short-Term Considerations
A 1000mg prednisone dose delivers a significant amount of corticosteroid to your system. Expect noticeable effects within hours. You might experience increased energy, improved mood, and reduced inflammation. However, be aware of potential side effects like increased appetite, leading to weight gain, and difficulty sleeping. Fluid retention can also occur, causing swelling in your ankles or face.
Monitoring Blood Sugar
Prednisone elevates blood glucose levels. If you have diabetes, monitor your blood sugar closely and adjust your insulin or oral medication as needed. Frequent checks are crucial, especially during the initial days of treatment. Consult your doctor for guidance on appropriate monitoring frequency and dosage adjustments.
Gastrointestinal Upset
Some individuals experience stomach upset, including heartburn or nausea. Taking prednisone with food can help mitigate these issues. If severe, speak to your physician; they might recommend a medication to protect your stomach lining.
Long-Term Risks and Management of Side Effects
Prednisone at 1000mg daily carries significant long-term risks. Monitor for osteoporosis, requiring calcium and vitamin D supplementation along with weight-bearing exercise. Regular bone density scans are recommended.
Increased blood sugar is common; frequent blood glucose monitoring is crucial, especially if you have diabetes or risk factors. Dietary adjustments and potentially medication adjustments are necessary.
High blood pressure frequently occurs. Regular blood pressure checks are vital. Lifestyle changes, such as a low-sodium diet and increased physical activity, should be implemented; medication adjustments may be needed.
Cataracts and glaucoma are potential eye complications. Regular eye exams are essential for early detection and treatment.
Immunosuppression increases infection risk. Practice good hygiene and avoid contact with sick individuals. Report any signs of infection immediately.
Weight gain and muscle wasting are common. Maintain a balanced diet, prioritize protein, and engage in regular exercise, adapted to your capabilities, to mitigate these effects.
Mood swings and insomnia are possible. Maintain open communication with your doctor and consider cognitive behavioral therapy (CBT) or other strategies for managing these.
Your doctor will develop a personalized tapering schedule to minimize withdrawal symptoms when reducing the prednisone dose. This is a gradual process to prevent adverse reactions.
Always discuss any concerns or new symptoms with your physician. They will help you manage side effects and adjust your treatment plan as needed.
Remember: This information is for general knowledge and does not replace professional medical advice. Consult your doctor for personalized guidance and monitoring.
Withdrawal and Tapering Strategies
Never abruptly stop prednisone. A slow reduction, called tapering, is crucial to avoid serious withdrawal symptoms.
Understanding the Tapering Process
Your doctor will create a personalized tapering schedule. This typically involves gradually decreasing your dose over several weeks or months. The exact duration depends on several factors, including your dosage, duration of prednisone use, and overall health.
- Example Schedule (Consult your doctor; this is not a prescription): A patient on 1000mg might reduce by 5mg-10mg per day or week, depending on the doctor’s recommendation and the patient’s response.
- Frequency of Dose Adjustments: Reductions might be daily, every other day, or weekly, depending on your individual needs and response.
- Monitoring Your Progress: Regular blood tests and check-ups are necessary to monitor your body’s response to the tapering schedule. Be prepared to communicate any side effects you experience.
Potential Withdrawal Symptoms and Management
Withdrawal symptoms can vary widely, but common ones include fatigue, muscle weakness, joint pain, nausea, and mood changes.
- Fatigue: Get adequate rest, avoid strenuous activity, and communicate fatigue levels to your doctor.
- Muscle weakness and joint pain: Gentle exercise and physical therapy may be recommended. Your doctor might suggest other pain management strategies.
- Nausea: Eat small, frequent meals and stay hydrated. If nausea is severe, inform your doctor.
- Mood changes: Consider support groups or counseling, as necessary. Open communication with your doctor is crucial in managing emotional well-being.
Remember: Closely following your doctor’s tapering schedule is paramount to minimizing withdrawal effects. Don’t hesitate to contact your physician if you experience any concerning symptoms. They are your best resource for adjusting the tapering plan as needed.